Hyperthermia is an overheating of the body that goes against the natural tendency of our temperature-regulation centre — the internal system that normally works to keep us in balance.
Unlike a fever, it isn’t triggered by pyrogens, and that’s why it doesn’t respond to standard fever-reducing medicines. One particular form is malignant hyperthermia, in which a dangerously high body temperature can occur as a severe adverse drug reaction — and it can also arise after taking certain drugs (e.g. Ecstasy).
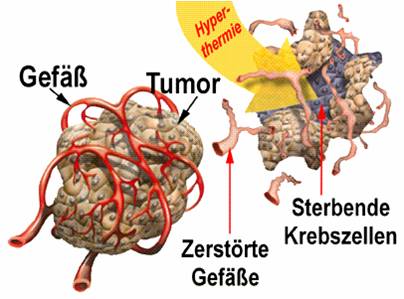
A deliberately induced rise in body temperature (therapeutic hyperthermia) is used, for example, in the treatment of cancer. Hyperthermia is especially used within alternative cancer approaches and in complementary oncology. By intentionally warming the body, it may, in individual cases, support a chemotherapy or radiotherapy that has previously been ineffective — or help it become effective in the first place.
There are different forms of hyperthermia. Broadly, the text distinguishes between whole-body hyperthermia, locoregional deep hyperthermia, and prostate hyperthermia. In whole-body hyperthermia, the entire body — with the exception of the head — is gently overheated using water-filtered infrared emitters. In this process, body temperature typically reaches between 39.5°C and 40.5°C. In locoregional deep hyperthermia, only the affected tissue or organ is overheated, to a maximum of 44°C. A particularly important approach is the treatment of the prostate using transurethral hyperthermia. Here, heat is combined with an electromagnetic field generated by radio shortwaves.
Source: Wikipedia
This is what doctors call regional hyperthermia: the deliberate, targeted warming of tissue — based on the idea that tumour cells can be damaged or die when heated to around 40 to 43°C. Unlike fever therapy, where the whole body is raised to fever temperature with the help of bacterial toxins, regional hyperthermia remains locally limited. In certain cancers — such as pancreatic cancer and malignant germ cell tumours, a rare type of cancer in children — this approach has shown promising results. And in bone and soft-tissue tumours, the so-called sarcomas, the benefit of hyperthermia has been recognised for some time. That is why statutory health insurance providers will cover the costs — provided the treatment takes place in clinics certified by the hyperthermia specialist society ESHO — and only then. “The chance that the tumour shrinks doubles when hyperthermia is combined with chemotherapy,” says Issels. “For patients, it’s a meaningful gain in both length of life and quality of life.” Experts are also placing their hopes in so-called thermosensitive liposomes: if contrast agents and medicines are enclosed in these tiny fat particles, the liposome shell only dissolves exactly where the tumour is being heated through hyperthermia — releasing the medication on the spot. “The chemotherapy is released precisely where it’s meant to do its main work,” says Issels. “That is the future.”
Source: https://www.spiegel.de/gesundheit/diagnose/hyperthermie-krebszellen-im-waermestress-a-909220.html
Who covers the costs if I decide to undergo hyperthermia treatment?
Before starting treatment, patients should clarify in advance whether their health insurance provider will cover the costs of hyperthermia. Since hyperthermia is currently not a standard treatment in Germany, insurers are not obliged to pay for it. In certain cases, however, they may agree to cover the costs as an individual case decision. Before reaching a decision, insurance providers usually review the specific circumstances under which the treatment is to take place — including the clinic, the medical indication, and how the therapy is integrated into an overall treatment plan.
A link to a very detailed explanation of this topic can be found here: https://www.krebsinformationsdienst.de/behandlung/hyperthermie.php